A disturbing incident involving a teenage girl has sparked widespread discussion across social media and health-focused communities, serving as a sobering reminder of how easily curiosity, misinformation, and silence around health topics can lead to serious consequences.
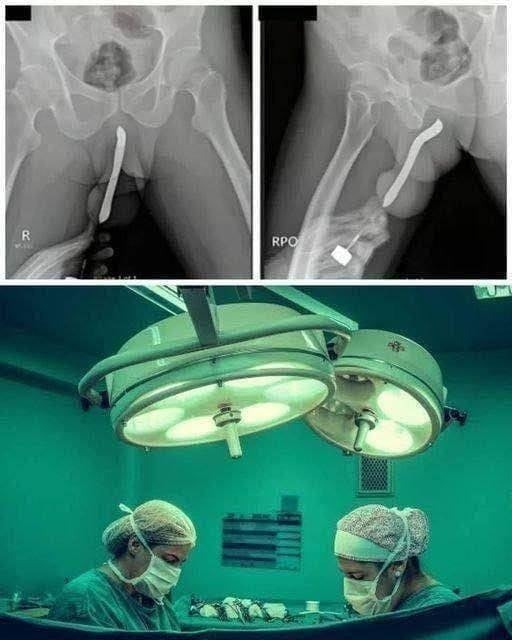
According to reports, the teenager was rushed to the hospital after attempting a dangerous experiment involving a common household object. She reportedly inserted a pen into her body, causing severe internal injuries that required immediate and urgent medical intervention. What may have begun as a moment of curiosity or impulsive behavior quickly escalated into a medical emergency. Doctors acted swiftly to assess the extent of the damage, stabilize her condition, and prevent life-threatening complications. Although medical professionals were able to intervene in time, the incident left both physical and emotional consequences that may take far longer to fully heal.
To protect the teenager’s identity and privacy, specific medical details have not been publicly disclosed. However, the broader implications of the case have extended far beyond the hospital walls. What initially appeared as a shocking and sensational headline has since evolved into a larger, more complex conversation about adolescent development, gaps in health education, digital misinformation, and the psychological vulnerabilities of young people navigating a hyper-connected world.
Medical professionals familiar with similar cases explain that injuries involving foreign objects inserted into the body can escalate rapidly. Objects not designed for internal contact can puncture delicate tissues, tear internal linings, and cause significant bleeding. In addition, they can introduce harmful bacteria, leading to serious infections. In some instances, complications such as internal perforation, abscess formation, or organ damage can occur. If treatment is delayed, the consequences may become irreversible or even fatal. For this reason, emergency responders treat such situations with extreme urgency and discretion, prioritizing stabilization and infection prevention.
Doctors working in emergency medicine and adolescent care note that teenagers are particularly vulnerable to high-risk behavior. Adolescence is a developmental period marked by intense curiosity, identity exploration, and a desire for independence. The brain’s decision-making and impulse-control systems are still developing, while curiosity and sensation-seeking tendencies are heightened. When natural curiosity intersects with limited anatomical knowledge, peer influence, or misleading online information, the results can be dangerous.
Health experts emphasize that the digital age has transformed how teenagers seek answers to sensitive questions. In previous generations, young people might have turned to parents, teachers, school nurses, or family doctors for guidance. Today, many adolescents rely heavily on social media platforms, video-sharing sites, online forums, and anonymous communities. While some online content can be educational and supportive, much of it is inaccurate, oversimplified, or deliberately sensationalized for attention. Viral “challenges,” poorly explained so-called experiments, and anecdotal stories can create the false impression that risky behavior is common, harmless, or even humorous.
In this particular case, online speculation suggests the teenager may have been influenced by curiosity about anatomy or by misleading information encountered digitally. Medical professionals strongly caution against ridicule or blame. Public shaming, they argue, only deepens stigma and discourages young people from seeking help when they need it most. Adolescents who fear embarrassment are significantly more likely to hide injuries or delay treatment, increasing the risk of serious complications.
The emotional impact of such an incident is often underestimated. Beyond physical recovery, teenagers may experience intense embarrassment, shame, anxiety, or guilt following a medical emergency tied to personal experimentation. The hospital environment itself can be overwhelming, particularly when the injury involves intimate areas of the body. Mental health support is frequently necessary to help young patients process what happened, cope with public or peer reactions, and rebuild their sense of self-confidence. Without proper psychological care, the emotional effects can persist long after physical wounds have healed.
Parents and caregivers are often left shaken by events like this. Many report feelings of shock, confusion, and self-doubt, questioning whether they missed warning signs or failed to have important conversations. Health professionals remind families that even attentive and caring parents cannot monitor every thought, question, or online interaction their children experience. Adolescents often explore sensitive topics privately, especially if they fear judgment or discomfort. Experts stress that what matters most is creating a household environment where discussions about bodies, boundaries, and health can happen openly and without shame.
Educators and healthcare providers widely agree that comprehensive, age-appropriate health education is one of the most effective tools for prevention. When young people receive accurate information about anatomy, bodily safety, consent, and medical risks, they are less likely to experiment in unsafe ways. Avoiding or delaying these conversations does not shield teenagers from curiosity; it leaves them vulnerable to myths, misinformation, and peer-driven speculation. Clear, medically accurate education empowers adolescents to make safer decisions and to recognize when something is dangerous.
Hospitals acknowledge that while cases involving foreign object injuries are not everyday occurrences, they are not unheard of. Emergency departments occasionally treat both adolescents and adults who underestimated the risks associated with inserting objects into the body. These cases reinforce the need for greater public awareness. However, medical professionals caution that awareness campaigns must be handled responsibly, without sensationalism that could inadvertently encourage imitation or amplify harmful curiosity.
Online reactions to the incident have varied widely. Many individuals expressed concern, empathy, and support for the teenager’s recovery. Others responded with shock humor, disbelief, or harsh judgment. Healthcare experts warn that mocking reactions can create a culture of silence around medical mistakes. Fear of public humiliation is one of the primary reasons individuals delay seeking medical attention after risky behavior, often worsening health outcomes.
Emergency medicine professionals emphasize a simple but critical message: if something goes wrong, seek help immediately. Hospitals and emergency rooms are spaces designed for treatment and confidentiality, not punishment or ridicule. Prompt medical care can mean the difference between a manageable injury and long-term damage. Delaying care out of embarrassment can dramatically increase medical risks.
The case has also renewed calls for greater accountability from digital platforms. Experts argue that algorithms designed to maximize engagement may unintentionally amplify sensational, risky, or misleading content. While personal responsibility remains important, many public health advocates believe platforms should invest more heavily in moderation, content warnings, and partnerships with credible health organizations. Improved digital literacy education is increasingly viewed as an essential safeguard, helping young people critically evaluate the information they encounter online.
At its core, this story is not about shock value or sensational headlines. It is about awareness, prevention, and compassion. It illustrates how quickly dangerous situations can arise when natural curiosity meets inadequate education and unfiltered digital content. It highlights the need for honest, ongoing conversations between teenagers and trusted adults. It underscores the importance of accessible, reliable sources of health information.
Medical professionals specializing in adolescent care hope that the attention surrounding this case will encourage families, schools, and communities to approach health education with openness rather than avoidance. Preventing similar incidents does not require fear-based messaging. Instead, it requires clarity, empathy, accurate information, and safe spaces for questions. Adolescents deserve guidance rather than judgment.
The teenager’s hospitalization serves as a powerful reminder that health education is not optional, embarrassment should never outweigh personal safety, and curiosity should be met with support instead of silence. While the incident itself is deeply concerning, the broader conversations it has sparked may ultimately lead to stronger communication, better education, and improved safeguards for young people navigating both their development and the digital world.